Dear patient,
We would like to provide you with some information so that you can optimally prepare yourself for the planned vascular access for blood-cleansing (dialysis).
General information:
You have been diagnosed with the need for dialysis treatment, which is usually carried out three times a week (cycle A: Monday, Wednesday, Friday; cycle B: Tuesday, Thursday, Saturday). In order to be able to guarantee blood-cleansing, you need a permanent vascular access. This vascular access represents your lifeline and ensures the vital blood washing.
Types of vascular access:
The method of first choice for such vascular access is the open surgical creation of a so-called arterio-venous fistula (AV fistula) on the forearm. Here, a short-circuit connection is made between an artery (oxygen-rich blood, high pressure) and a superficial, easily accessible vein (oxygen-poor blood, low pressure). Due to the low pressure in the vein, the blood flows with little resistance from the artery into the vein, which then enlarges in diameter and thickens in the area of the vein wall in the following weeks and months. This process is called maturation (maturation). This enlarged vein (so-called shunt vein) is easily visible and palpable and can therefore be easily pricked with needles during blood washing.
The arm used is primarily the non-dominant arm, i.e. the left arm in the case of right-handers (and vice versa). Maturation takes between 8 and 12 weeks, depending on the initial diameters of the artery and vein. Therefore, the ideal time to create an AV fistula is when the patient does not yet need dialysis, but will foreseeably need it in the medium term.
If the artery and/or vein on the forearm is not suitable for the creation of an AV fistula because it is too slender or pre-diseased (vascular calcification/atherosclerosis), the short-circuit connection can also be made in the crook of the arm, on the upper arm or on the thigh.
In some cases, there is no suitable vein in the entire arm, but there is a suitable artery. In these cases, a plastic prosthesis inserted under the skin can be connected to an artery and vein and then used for blood washing. Maturation is usually not necessary. However, the surgical wounds should have healed before being used for the first time in blood-cleansing.
Both the AV fistula and the plastic prosthesis are associated with increased cardiac stress due to the greatly increased backflow of blood to the heart. In such cases, a so-called atrial catheter can be inserted. A catheter is inserted into a large vein leading to the heart through two small incisions in the neck and below the collarbone. The tip of the catheter comes to rest in the right atrium of the heart. An atrial catheter can be used directly after the operation, which is why it is also very suitable if dialysis is necessary at short notice and vascular access to the arm has not yet been planned. It can also be used to bridge the several-week maturation period of an AV fistula.
In principle, any vascular access avoiding foreign material (plastic) should be favoured as it offers considerable advantages in terms of avoiding infections as well as durability.
Consultation with your specialist:
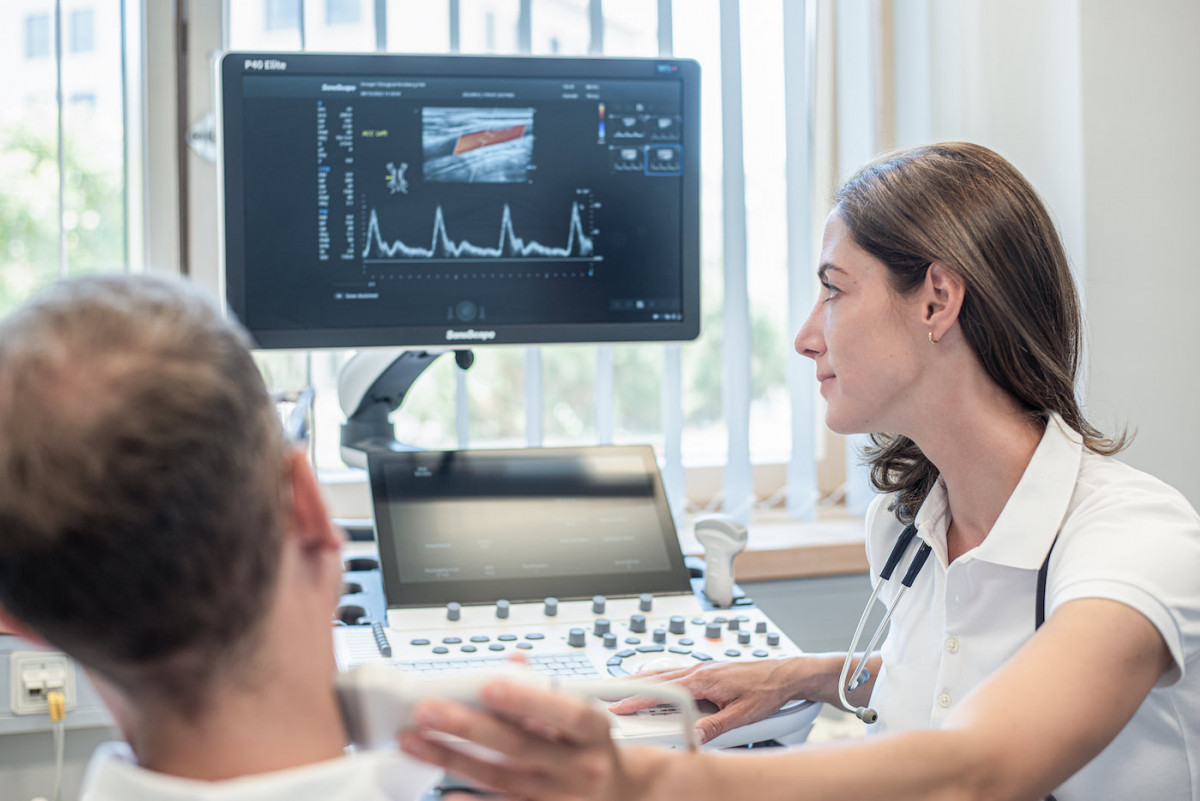
During a detailed and confidential consultation - including an ultrasound examination of the veins - you will learn everything you need to know about the necessary preparation, the course of the operation, aftercare and possible risks and complications of the planned procedure. If you have any further questions, you are of course welcome to contact us again.
You should be able to answer the following questions:
Have you had dialysis access in the past? If so, when and what exactly was done?
What is your health status? Tell us about any illnesses, accidents or chronic conditions. Is there any heart disease? Do you have an acute infection (COVID, hepatitis, flu)?
Do you regularly take medication? If so, which ones and in what dosage?
Are you taking medication to thin your blood? If yes, which ones and in which dosage?
Do you suffer from allergies?
Do you have any blood clotting disorders?
Pre-inpatient preparation:
Before your operation, you will receive prescriptions by post for a blood test and a COVID-PCR test (may change depending on the current infection situation). You will be informed by the anaesthesiology department of the hospital about an appointment for anaesthesia information. The COVID PCR test must be carried out 24-48 hours before your admission to hospital. Please bring the negative result with you as a printout or digitally to your admission to the hospital. If the test is positive, we ask you to stay at home and inform us immediately by telephone about the positive test result. We will organise an alternative date for your operation as soon as possible.
We will also send you a surgical information sheet about the surgical procedure. We kindly ask you to read and complete this form carefully. Please be sure to bring the information sheet with you to the operation. If there are any questions, we will of course clarify them before your operation.
Important: If you are planning to have a vascular access in your arm, blood samples must not be taken from the affected arm in the weeks before the operation!
Inpatient stay:
Every type of dialysis access is performed in our hospital under inpatient conditions and in cooperation with the doctors of the Department of Nephrology. The inpatient admission usually takes place on the day before the operation, unless the patient is already in hospital due to the kidney disease.
The creation of a vascular access in the arm can be carried out under general anaesthesia or regional anaesthesia (plexus anaesthesia), depending on the existing pre-existing conditions and the patient's wishes. In the latter case, the patients are awake and only the affected arm is under anaesthesia, so that you do not feel any pain. You decide which method should be performed on you together with us and the anaesthetist.
An atrial catheter is usually inserted under general anaesthesia.
If an AV fistula is inserted, it is usually possible to discharge you the following day due to the surgical wounds. If you have had an atrial catheter implanted, its proper functioning will be checked before discharge in the course of an initial blood-cleansing.
After the insertion of a plastic prosthesis or after corrective surgery on existing dialysis lines, you should expect a stay of 5-7 days. Depending on whether the doctors of the Department of Nephrology have planned further examinations and treatments for you, the inpatient stay may be longer.
Aftercare:
You will receive prescriptions from us for plasters, painkillers and, if necessary, an outpatient nursing service to carry out the daily dressing changes.
A wound check including the pulling of the skin sutures will take place in the consultation hours of the surgeon who operated on you, usually on the 10th-12th day after the operation. You will automatically receive the appointments before discharge.
As a rule, showering is only allowed after the skin stitches have been removed!
Should you experience fever, chills, severe pain or fluid secretion in the wound area during the first few days after the operation, please call our office and come in for a check-up.
The operated arm must be rested for about two weeks.
Blood pressure measurements and blood samples must not be taken from the operated arm!
Due to the swirling blood flow in the shunt vein, a characteristic "buzzing of the shunt vein" occurs already initially after the creation of an AV fistula, which can be felt even by laypersons without prior medical knowledge.At home, the buzzing of the shunt vein should be checked several times a day by you or your relatives in order to be able to recognise possible problems at an early stage.
The maturation of the shunt vein can be accelerated by muscle work of the hand, for example by repeatedly squeezing a rubber ball. Don't worry, you can't do anything wrong here, too much exercise is not possible!
The vascular access is regularly assessed by us as well as your attending kidney specialist (nephrologist). Together we will decide when the vascular access can be used for the first time.
Despite correct puncture technique and optimal care of the vascular access, surgical corrections are often required over time due to the constant manipulation during dialysis.
Constrictions (stenoses) and occlusions (thromboses) of the shunt vein or the plastic prosthesis can occur, which have to be treated surgically or by means of catheter techniques (angioplasty).
Occasionally, dilatations of the shunt vein (aneurysms) can occur, which do not have to be corrected in every case. However, correction is necessary if the dilatation has reached an appropriate size or if there is prolonged post-operative bleeding after blood washing.
In case of very high blood flows in the shunt vein, a so-called throttling may become necessary in order to avoid a circulatory disorder of the hand and/or an overload of the heart.
Our primary goal is always to preserve an AV fistula for as long as possible, since your body's own available vein material is limited and atrial catheters and plastic prostheses must always be considered secondary.
Through our many years of work at highly specialised shunt centres in the past, we have been able to acquire extensive and excellent expertise in the surgery of dialysis accesses.Any problem with your dialysis access will be solved by us in close and valued cooperation with our colleagues in renal medicine around the clock and as quickly as possible in order to be able to guarantee your vital dialysis again!
 Deutsch
Deutsch  English
English  Français
Français